Are you wondering why they’re changing how skilled nursing facilities (SNF) are being reimbursed by Medicare? Payments are always under intense scrutiny and changing the process of payments has been a long discussion. There are deep concerns around therapy minutes driving high reimbursement groups and many assessments scoring in those upper RUGs were at or within 5 minutes of the RUG minute threshold. The Medicare Payment Advisory Commission (Med PAC), the Centers for Medicare and Medicaid Services (CMS), and the Department of Health and Human Services Office of the Inspector General (OIG) all discussed the need for a new reimbursement model for Medicare Part A in a SNF – one that is not driven by the amount of therapy services delivered. The discussion concluded with the Med PAC, CMS, and OIG believing that the current SNF Prospective Payment System (PPS), which is based on Resource Utilization Groups (RUGs), is wrongfully incentivizing the utilization of therapy services and neglecting the fact that medically complex residents often need more complex care that is not therapy related.
All in all, the IMPACT Act of 2014 requires that the post-acute care sector take on a unified payment system driven by cross-setting measures by 2024. Over the last several years, SNFs have seen several payment models. As you are aware, October 1st marks a new payment model referred to as the Patient Driven Payment Model (PDPM).
Coming back to the question, “Are you wondering why they’re changing how SNFs are being paid?” The best way to begin to explain this is to compare the current payment plan RUG-IV to PDPM.
What is Resource Utilization Groups (RUG-IV)?
RUG-IV is a patient classification system for skilled nursing patients used by the federal government to determine reimbursement levels. This method is stemming from the SNF PPS FY2012 Final Rule and was previously RUG-III. Payment is determined by categorizing patients into groups based on their care and resource needs. This system primarily determines payment by the number of therapy minutes. Which doesn’t fully consider the wide range of clinical characteristics that influence the relative resource use of residents.
What is Patient Driven Payment Model (PDPM)?
PDPM is a case-mix group (CMG) reimbursement method that focuses on clinically relevant factors rather than volume-based services or RUG-IV codes. It improves payment accuracy and appropriateness by focusing on the patient rather than the volume of services provided. PDPM focuses on the unique, individualized, and characteristic needs, and goals of each patient, and significantly reduces administrative burden on providers to improve targeting of resources to beneficiaries with diverse care needs. Payments are calculated through patient CMG scores meaning with PDPM therapy minutes are no longer the driving force for payments.
What are the differences between RUG-IV and PDPM?
Classifications from RUG-IV assigns patients to payment classification groups, called RUGs, within the payment components, based on various patient characteristics and the type and intensity of therapy services provided to the residents.
- Rehabilitation Plus Extensive Services
- Rehabilitation
- Extensive Services
- Special Care High
- Special Care Low
- Clinically Complex
- Behavioral Symptoms and Cognitive Performance Problems
- Reduced Physical Function
Classifications under PDPM have six payment components that are utilized to derive reimbursement. Utilizing clinically relevant factors, rather than volume-based service for determining Medicare reimbursement. Patient characteristics are used to assign residents to CMGs across the payment components to derive payment. PDPM also adjusts per diem to reflect varying costs throughout a patient’s stay.
Nursing classification –
The total number of nursing case-mix groups (CMGs) has been reduced by decreasing distinctions based on functions where the resource utilization costs did not differ. PDPM is consolidating 43 nursing RUGs into 25 nursing CMGs.
SLP Classification –
Speech-language pathologist (SLP) classification is based on three elements in PDPM:
- Diagnosis of the clinical category using the ICD-10-CM and ICD-10-PCS recorded in MDS item I8000. The diagnosis code should represent the main reason the resident requires skilled nursing care. For speech, there are only two clinical category options: Acute Neurologic and Non-neurologic.
- Determine if the resident has the presence of swallowing disorder or mechanically altered diet using item K0100A through D and K0510C2.
- Consider and decide if the resident has cognitive impairment. Cognitive impairment is based on:
The BIMS and CPS as documented in Section C of the MDS: Cognitively Intact, Mildly, Moderately, and Severely Impaired.
If the resident has one or more SLP-related comorbidities such as:
a) The BIMS and CPS as documented in Section C of the MDS: Cognitively Intact, Mildly, Moderately, and Severely Impaired.
b) If the resident has one or more SLP-related comorbidities such as:
- CVA/TIA/Stroke
- Hemiphlegia/Hemiparesis
- Trach
- Vent
- Laryngeal Cancer
- Apraxia
- Dysphagia
- ALS
- Oral Cancer
- Aphasia
To determine the overall score, CMS combined the clinical category, cognitive impairment, and present of SLP-related comorbidity into a single predictor. Using the SLP CMGs along with the presence of Mechanically Altered Diet or Swallowing disorder, the provider can determine the results using the 12 SLP CMGs.
NTA Classification –
Non-therapy Ancillary (NTA) includes services that are considered to be expensive or above and beyond the typical nursing cost, for example: transplants, IV meds, ventilator, chemotherapy, HIV/AIDS, opportunistic infections, transfusions, and more. In PDPM, NTA CMGs are determined from the total NTA score using the PDPM Calculation Worksheet.
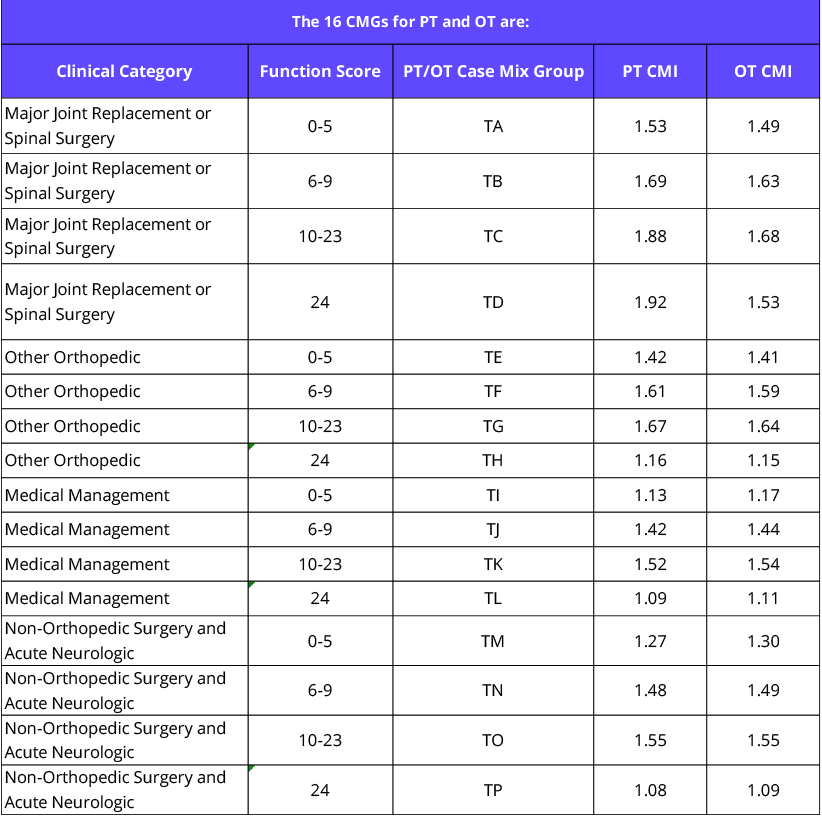
PT/OT Classification –
PDPM reclassified the RUG-IV categories into 16 possible CMGs broken down into two components:
10 Clinical categories
- Major Joint Replacement/Spinal Surgery
- Orthopedic Surgery (Except Major Joint Replacement or Spinal Surgery)
- Non-orthopedic Surgery and Acute Neurologic
- Other Orthopedic (non-surgical orthopedics & musculoskeletal)
- Medical Management (medical management, acute infections, cancer, pulmonary, cardiovascular/coagulation, acute neurologic)
Functional scoring that is based on the Eating, Oral Hygiene, Toileting Hygiene, Sit to Lying, Lying to Sitting on Side of Bed, Sit to Stand, Chair/bed-to-Chair Transfer, and Toilet Transfer Admission Performance. Once those scores are gathered, the residents walking abilities are scored. Each performance function is scored on a range of 0-4 scale. The average function score of the daily activities and the average walking score, the facility will then round the sum of those two scores which will result in the PDPM Function Score for OT/PT Payment. The average PDPM Function Score for OT/PT Payment ranges between 0-24.
Summary
Over the next several months, we will provide more information on PDPM and best to prepare your facility, such as our recent Phase I through PDPM: Future Challenges and Opportunities. Given the depth of changes coming with the reimbursement model changes, we know that many of you are busy preparing and evaluating the clinical capabilities, MDS coding, and gaining an understanding of the strategic needs of the new payment model. These changes are a major new opportunity for SNFs to succeeding in a value-based world.

