Today we are talking with Laurie Laxton of ABILITY Network, an infection prevention expert, to discuss the best processes for infection prevention, control, and surveillance and help you formalize and upgrade your Infection Prevention & Control programs.
Infection Prevention & Control Programs
Infection Prevention and Control (IPC) is the practice of preventing or stopping the spread of infections in a healthcare setting. It is long-term care facilities’ regulatory solution to avoiding infections in their residents and health workers community.
It’s always been important, but especially during the COVID-19 pandemic, IPC is one of the most relevant care programs at every single healthcare facility especially those serving vulnerable or senior communities often found in long-term care.
Nursing homes often demonstrate a consistent lack of enforced IPC programs and Infection Control standardized policies that protect their residents. However, the government owns part of the blame. For years, the CMS has missed the opportunity to push care providers to develop Infection Prevention basic policies and specialized training.
The consequences of this have been tragic in nursing homes and SNFs, being the cause of millions of cases of disease in infection outbreaks across the country.

The presence of an empowered Infection Preventionist and adequate EHR solution to continually monitor all the community’s contamination signs and prevention procedures are crucial to providing safe and efficient long-term care.
Since the COVID-19 pandemic startled the long-term care industry, this has become more urgent than ever. IPC programs have overlapped nursing home management priorities, but the government is also waking up and getting more involved in monitoring the effectiveness and processes of these programs, both through punishments and rewards.
HHS Funding Goes to Those With Top Infection Control Performance
On October 28, the Department of Health and Human Services (HHS) announced allocating about $333 million in payments among 10,000 nursing homes that managed to improve their COVID-19 infection and death rates over the last two months.
The initiative is motivated by the industry’s need for robust Infection Prevention and Control programs. By providing these performance-based incentives and making new Infection Control training resources available, the CMS aims to consolidate effective Infection Control policies and roles that generate substantial progress in long-term care’s fight against COVID-19.
More specifically, HHS will evaluate nursing homes based on two criteria:
- Infection Criteria
- Mortality Criteria
Back in August, HHS already distributed $5 billion to nursing homes. While half of it promoted COVID-19 testing, facilities staffing, and personal protective equipment needs, the other half’s allocation was also based on performance.
Infection Control as CMS’s Central Priority
The CMS is closely tracking nursing homes’ performance based on their weekly National Healthcare Safety Network (NHSN) data to ensure that facilities introduce robust surveillance programs and Infection Control programs that meet all of the high-quality IPC program elements.
Nursing homes must gather, report, and utilize accurate and verifiable surveillance data using standard Infection Control definitions to comply with the NHSN requirements for a legitimate IPC.
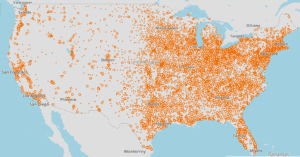
You can refer to the NHSN’s database for a detailed breakdown of the CMS Nursing Home COVID-19 Public File.
There you’ll find links to resources as well as useful graphs and maps such as density of nursing homes across the country.
Reporting Requirements and Staff Testing
Knowing what the current requirements are for infection reporting and testing is an important part of maintaining regulatory compliance. But how do you know when to test staff and residents?
CMS Updates COVID-19 Testing Methodology for Nursing Homes is a great resource to bookmark to make sure you’re up-to-date on regulations.
In addition, CMS has produced this in-depth document detailing Measures for Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAIs) Requiring Hospitalizations
As part of their strict involvement, the administration is not only compensating care providers but also flagging them or locking them down when necessary based on NHSN’s reporting data on:
-
- Smart and consistent testing of staff and patient or residents
- Utilization of a standardized definition of infection prevention and control criteria
- Infection Preventionists and surveyors feedback
- F-Tags from Healthcare-Acquired Infections (HAI)
Survey F-Tags Associated with Infection Control
Infection Control Focused surveys during the initial pandemic and beyond have several key areas that have neem reported to be emphasized. These include
- Documentation of staff education on Policies and Procedures, infection control practices.
- Areas where improper infection control practices have been cited (i.e. not properly donning PPE, breaks in aseptic technique, etc.)
The most common F-tags related to infection control include:
- F-880
- F-881
- F-884 New during PHE pertaining to NHSN reporting
- F-885 New during PHE pertaining to family notification of COVID-19 cases
- F-886 New pertaining to testing requirements
- Other F-tags are not always considered but also tied to infection prevention and control programs
F880 to Regulate Healthcare-Acquired Infections
Nursing homes have always been compelled to develop a thorough understanding of critical F-Tags and adopt emergency preparedness requirements to ensure they avoid steep fines following Infection Control-focused surveys.
Yet, since the pandemic became the industry’s most threatening and time-sensitive matter, the CMS is exclusively prioritizing HAI’s monitoring. As Infection Control rises in the regulatory spotlight, the government centers its new survey process on the new F880 Tags, based on the attribution of Healthcare-Acquired Infections.
Of course, CMS regulations change frequently. Here is the newly proposed SNF QRP Measure surrounding HAIs in Skilled Nursing Facilities
What Do Surveyors Focus on for The F880 Tag?
- Hand hygiene
- Appropriate Personal Protective Equipment (PPE)
- Transmission Based Precautions
- Laundry
- Overall IPC program quality compliance
This F-Tag’s uprising and HHS’s incentive programs help the government enforce effective infection prevention in nursing homes through increasingly stringent IPC program establishment and maintenance requirements. Measures center on providing a safe, sanitary, and comfortable environment and preventing the development and transmission of the COVID-19.
What Exactly is an Infection Preventionist?
Infection Preventionists ensure healthcare providers and residents follow Infection Prevention best practices and meet surveillance quality requirements.
In 2016, the CMS announced IPC programs’ mandatory nature within nursing home regulations. Since November 2019, this requirement has focused on compelling facilities to nominate an on-site Infection Preventionist.
Due to limited resources and in some cases because of in-house expertise, this role is often taken on as an additional duty by nurses, epidemiologists, public health professionals, microbiologists, doctors, or other health professionals from the facility.
What to Look for in an Infection Preventionist
Infection Preventionists aren’t required to be certified or nurses, but the government demands at least essential epidemiology background and proper training on Infection Prevention and Control.
To hire or select the right Infection Preventionist from your team, some professional and attitude requirements should be met to ensure your facility’s IPC program efficiency.
- Strong communication and leadership skills. The right Infection Control surveyor has to work hand-in-hand and collaborate with doctors, administrators, and other authorities.
- Attention to detail. He or she will need to be able to identify potential breaks in Infection Control, sterile techniques, and on-site policies and procedures.
- Organized and thorough problem solver. An efficient Infection Preventionist would ideally be confident and interested in designing and writing policies and procedures for all potential infections.
- Not be afraid to speak up. This is likely the most important trait of an effective Infection Preventionist. Your organization and community’s safety is in their hands, and they have to be committed to reporting issues when they arise.
What Does an Infection Preventionist Do?
- Tracks infection patterns within the facility
- Survey practices
- Educates teams
- Provides advice and recommendations
- Compiles Infection Control data for the NHSN
- Designs complying policies and procedures
- Coordinates with local and national public health agencies
What Must Their IPC Program Achieve?
- Hand Hygiene
- Regulated Immunizations
- Proper Medication Management
- Catheter Devices Correct Application
- Safe Infection Control Practices
- Right PPE Usage
- Correct Room and Equipment Cleanness
What Training is Available for an Infection Preventionist?
Once you’ve selected the right person for the job, you’ll need to ensure that they have the resources and knowledge to be effective in their role. Fortunately, there are plenty of free online resources you can utilize.
CDC’s Infection Control Training and Education Webinars
To consolidate the implementation of coordinated IPC programs in nursing homes across the country, the CMS and CDC teamed up to promote the release of a series of More than 20 specific training topics with free learning modules and other training resources.
There you will find the tools and resources needed to educate healthcare providers on best practices to improve patient safety, such as free Webinars with continuing education.
These training materials aim to teach Infection Control best practices and empower Infection Preventionists’ role as the facility’s arm on surveillance programs.
QSEP CMS-CDC Training for Nursing Homes
This COVID-19 targeted certificate includes both trainings for front-line staff and administrators and it’s scenario-based.
How to sign up for the QSEP CMS-CDC Targeted COVID-19 Training
QIO Series and Certificates on COVID-19 Prevention Fundamentals
The Quality Improvement Organizations (QIO) provides a Comprehensive National Nursing Home Training Series in partnership with the CDC and CMS to deliver coronavirus prevention-centric training materials and live Q&A sessions with on-completion Participation Certificates in the following areas.
- Establishing an IPCP in a Nursing Home
- Is Your Nursing Home Ready to Handle COVID-19?
- COVID-19 Surveillance: NHSN Mandatory Data Collection
- COVID-19 Testing
- Cohorting Strategies
- Cleaning Environmental Surfaces and Shared Equipment
- Creating a COVID-19 Recovery Center
- PPE Strategies for COVID-19 Care
- Accepting New Patients During an Active Pandemic
- Telehealth in Nursing Homes
- Transparency: Resident and Family Notification
- Clinical Care: Managing COVID-Positive Residents
- Managing Staffing Challenges
CDC’s Project Firstline
CDC’s new infection control training collaborative provides innovative content designed to engage, innovate, and effectively train millions of frontline U.S. healthcare workers in Infection Control.
- COVID-19 Infection Prevention and Control
- Keep COVID-19 Out!
- COVID-19 Monitoring Residents
- COVID-19 PPE
- COVID-19 Environmental Cleaning
- COVID-19 Hand Hygiene
Antibiotic Stewardship
On October 9, 2020, the HHS released information on a new national action plan for combating antibiotic-resistant bacteria in 2020-2025
The CDC offers an interactive web-based program designed to help clinicians optimize antibiotic use to combat antibiotic resistance and improve healthcare quality and patient safety.
Take the Antibiotic Stewardship Training Series here
Electronic Solutions for Infection Control
Depending on manual methods to identify potential Healthcare-Acquired Infections within nursing homes can be extremely challenging and unreliable. Your staff is busy and no one can be perfect all the time.
Charting reviews, entering data, and looking for correlations is impossible to manually coordinate in mid-sized long-term care organizations and is highly susceptible to human error.
I’ve literally seen exit maps of the building photocopied in highlighter pens to highlight where the various infections are in the rooms.
Let’s say that a nurse forgot to highlight a room of somebody who had an MDR, which is a MultiDrug-Resistant organism. If they forgot to highlight it in a color, when you’re doing it manually, you have the risk of human error. “I forgot to color that room yellow.” Well, that patient discharges and the next one comes in, and he ends up with the same infection.
Electronic solutions streamline your health records management and Infection Control monitoring. A computerized system’s speed and efficiency overlap human capabilities to sort through the interoperability and real-time data filtering nursing homes require to comply with CMS’s regulations and your IPC program demands.
An EHR solution provides a more proactive Infection Prevention and Control approach compared with traditional techniques when collecting and coordinating resident data to stop or prevent infection outbreaks.
Learn More about the benefits of an EHR
EHR-Supported Surveillance Challenges
Introducing an electronic solution into your healthcare processes, data operability, and continuum of care management can be challenging and get a little pushback for its implementation affecting processes in the short-term.
But there’s no doubt about it, in 2020 healthcare teams need to learn new software, and many operational systems must change and upgrade to automate data management and standardize quality control practices. You just can’t operate effectively and stay competitive without it.
And nursing homes can’t ensure Infection Control coordination without automatic data management systems, especially during unexpected events, like our current pandemic. No IPC program can entirely prevent HAIs during a pandemic without properly standardizing Quality Assurance practices and tracking infection patterns facility-wide.
EHR computerized reminders to providers at the point of care lead to a 6.1% to 28.4% increase in preventive health programs.
NetSolutions QA reporting and documenting modules improve and update your facility’s Quality Measures and enable your Infection Preventionist to overcome the challenge of meeting CMS requirements to qualify for performance-based incentives.
The investment of your time in NetSolutions EHR upfront yields time-saving solutions on the back-end. Cloud-based solutions make your data and operating systems available and accessible for your teams, eliminating handwriting, filing, and pulling charts. You have access to modules to standardize report content while ensuring proper actions are taken and crucial data is captured to prevent and control infection breaks at the point of care.
Our interactive and user-centric training material and customer support assist your staff to tailor the system to your facility’s demands to begin streamlining your Infection Control program as soon as possible.
Learn how our Quality Assurance Module provides better Infection Control documentation and reporting.
How Can an EHR Enhance Your IPC Program?
Automate Your Data Surveillance
NetSolutions EHR analyzes your data by identifying abnormal distributions of variables from large interrelated databases.
Our EHR requires one-third to one-sixth the amount of time required by standard surveillance methods to screen potential outbreaks and find and report endemic HAIs.
With the current emphasis on mandatory reporting of HAI and CMS requirements to perform facility-wide surveillance, NetSolutions’ customer-driven EHR provides a unique opportunity to support the shift to automated surveillance strategies, allowing Infection Preventionists to minimize time spent finding HAIs and to maximize time spent preventing them.
Enhance Your IPC with Real-Time Data
To support your IPC program, you can customize your EHR to incorporate patient-specific clinical data such as laboratory or microbiology information along with diagnostic, demographic, and clinical guidelines. The software allows several decision support modes, including alerts for critical laboratory values and recommendations for best antibiotic practices.
NetSolutions’ communication and notification features enable better care plan coordination and timely notification of critical patient data to keep all your teams updated in Infection Control matters.
You can even customize automated alerts that specify the need for isolation and a negative-air room for a patient that is suspected to be infected.
NetSolutions’ Partnership with Infection Watch
NetSolutions integrates with ABILITY Network’s Infection Watch system to provide nursing homes with access to relevant, actionable data to rapidly identify infection outbreaks and establish the most efficient and regulatory prevention measures in your operations.
The integration connects directly with your residents’ EMRs to coordinate demographic information when pulling MDS assessments enabling Infection Watch to pull all NetSolutions’ demographic and medical records anytime an infection is entered.
Infection Watch ensures your Infection Prevention and Control program has the tools to improve infection surveillance and meet CMS requirements while improving residents’ outcomes.
- Streamline Infection Surveillance: Save time and resources identifying infection-related sentinel events and detecting outbreaks. Focus your IPC on prevention, intervention, and performance improvement efforts.
- Easily Meet Regulatory Compliance: The application helps your facility fulfill reporting requirements and avoid survey deficiencies and monetary penalties.
- Track and Trend Infections: Data interoperability allows you to identify problem areas and initiate corrective Infection Control measures quickly.
- Set Alerts and Notifications: Get the data you need automatically delivered so you can stay on top of infection surveillance.
Learn More About ABILITY Network’s Infection Watch System
Let’s Streamline Your IPC Together
Give us a call at (877) 290-3296 or schedule a consultation, and we can go through your specific IPC needs together.
Who is Laurie Laxton?

Laurie Laxton, RN,BSN,CCFA,RAC-CT,IP-BC
UCLA nursing graduate, specializing in Operating Room. Then as Nurse Coordinator of the UCLA Hand Center, and later, the Hip and Pelvic Reconstructive Division of the Good Samaritan Hospital, Los Angeles, Laurie was involved in cutting-edge technology and care. In the late 1990s, Laurie started a consulting business advising school districts and day camps on CPR, First Aid, medication administration, care planning, and incident reporting. In 2009, she became a Nurse Auditor, contracting with three national firms to conduct hospital and skilled nursing facility audits in several states and later obtained certification as a clinical financial auditor. In 2017, she pursued board certification in Infection Prevention. Currently, she is Clinical Education Program Lead at the ABILITY Network, an industry-leading software company that offers products to assist with Infection Prevention and Control, Quality improvement, risk reduction, and correct billing practices for the long-term care, acute care, and home health industries.
About ABILITY Network:
Guided by a mission to help, ABILITY, an Inovalon company, is a leading information technology company helping healthcare providers and payers simplify administrative and clinical complexity by enabling data-driven improvements in healthcare.
Through specialized, easy-to-use applications, and data analytics that work together, customers of all types and sizes across the continuum of care – rely on ABILITY to help optimize reimbursement, care quality, and staffing.

Transcript
Jason Long
Hello everyone. Welcome back. My name is Jason Long and I am the general manager at Cantata Health’s NetSolutions division. And I’m here today with Laurie Laxton. I’m going to read your credentials out real quick Laurie. RN, BSN, CCFA, RAC-CT, IP-BC, and you’re the Clinical Education Program lead at ABILITY. Did I get all that right?
Lauri Laxton
Yes.
Jason Long
All right. And today we’re going to be talking about Infection Prevention, Infection Preventionists, Electronic Systems, Incentives for Payments, and then some stuff that the government is doing, actually just released minutes ago.
Lauri Laxton
Yeah, coincidentally, yeah.
Jason Long
So tell me about yourself. How did you get into this? How did you become…how did you get so many letters behind your name?
Lauri Laxton
Well, you know, that’s one nice thing about nursing, you can go into all kinds of different areas. And so, when I graduated from UCLA, I was originally an Operating Room Nurse. And then I got into Nurse Coordinating. And so I was at UCLA for quite a few years. And then I dabbled in School Nursing when my kids were little, and I was a Camp Nurse. And when I was a School Nurse, I had to work with Incident Reporting and things like that, that also we have to do in the long-term care field. And then, about 11 years ago or so, I became a Long-Term Care Auditor. So I used to audit Skilled Nursing Facilities for some of the larger external companies. And I learned a lot about how Skilled Nursing Facilities are run. And then, about five years ago, I was approached to take on a position here at ABILITY Network, where I educate nurses in Nursing Homes, on MDS Assessments and Infection Control, and things like that. So that’s why there are all those letters. I’m a certified Medical Auditor, I’m also an Infection Preventionists, board-certified. And so, getting that additional training, it helps me when I go to train customers in different areas. I am very familiarized with the requirements and the things that they have to do in their day-to-day jobs.
Jason Long
Gotcha. Infection Preventionists are what we need a lot right now.
Lauri Laxton
Yeah. Yeah.
Jason Long
Yeah. So can you explain what is an Infection Preventionist? And what nurses can do to learn more about that?
Lauri Laxton
Well, a few years back, the CMS had a final rule that they rolled out in several phases. It started in 2016, where they said the Nursing Homes had to have an Infection Control Program. And then they rolled out you had to have an Antibiotic Stewardship Program. And then in November of 2019, you had to have an Infection Preventionist on-site, or at least a contracted with you to manage your Infection Prevention and Control program. And so, these Infection Preventionists actually wear many hats. Almost every one of them that I’ve met, they’re not only the Infection Preventionist, but they might also be the Director of Nursing, and they’re having to take on several roles in the building. The government has said that they have to get training in Infection Prevention and Control. You don’t have to be a nurse to be an Infection Preventionist you do need at least some kind of epidemiology background or something so that you understand the principles of an Infection Prevention and Control program. And then, CMS says that you need to have this person trained in Infection Control. And they don’t have to be certified. There are programs that CMS and CDC have rolled out that they can take modules. There’s the Infection Prevention, a series of modules, it’s about 23 modules. They’re very scenario-based, and they teach him how to do it. And then during the pandemic, CDC and CMS teamed up again and did more training for Infection Preventionists on a little more COVID specific. And then on top of that, the QIO’s in the various regions. They’ve been holding some fantastic webinars since May, that are all free. I think I provided NetSolutions with some links that you can share with the customers on how to get to all these. But boy, that QIO series has been really good too focus in particular areas each week, and it’s all recorded and so you can go back and listen to them.
Jason Long
What kind of person do you think makes the best Infection Prevention?
Lauri Laxton
They need to have a strong leadership background. They can’t be afraid to speak up. And identify breaks and sterile technique breaks and Infection Control policies and procedures. They also need to be somebody who is good at and likes to write a lot of policies and procedures, because you’ll have to write a lot of them for all the different types of infections, you have to be interested in all of the different types of infections, so that you can stay up on it and what needs to be reported what doesn’t. They also need to have a little basic understanding, and willingness to work with the doctors, with regards to antibiotic stewardship, which can be challenging as well.
Jason Long
So, is there a central location that people can go to for a list of best practices policy guide when they’re working in their facility? So, maybe just a set of SOP (Standard Operating Procedures) or policies?
Lauri Laxton
Well, I guess I would start with the final rule, the State Operations Manual, it will tell you what you have to, at a minimum, have in place to be an Infection Preventionist. And then from there, I really do believe that those training modules that I mentioned, would be they’re excellent, they’re a good place to start. And then your local QIOs (Quality Improvement Organizations) and the various State Public Health Departments have a lot of available tools at your disposal as well. That will help you in running certain areas of those Infection Control programs and assist you when you need help.
Jason Long
Okay, sounds good. Sounds good. So, moving on from Infection Preventionist. Tell me a little bit about the surveillance of prevention of infections?
Lauri Laxton
Yeah, so you have an Infection Prevention and Control program, they’ll often say, and they call it an IPC program. And surveillance is really just an element of an Infection Prevention and Control program. But I feel it’s the most important element. Because if you don’t have robust surveillance, how are you going to know what your baseline infection rates are, if you have problems in certain areas and things like that, so, and also surveillance programs are a 365 day a year, daily, it’s not that you just have it once a year. You do a little data analysis, and you call it a day, you got to constantly have feedback. So you’ll grab the data, you’ll see the tracking and trending, and then you have to figure out a way to disseminate that information out to your staff, where you find lack in process, person controls, and things like that.
Jason Long
So, right now, for so many facilities, funding is a huge issue. Can you tell me about what aspects are tied to the funding from CMS for surveillance?
Lauri Laxton
Well, you alluded at the beginning of this call that there is a new incentive program that just rolled out today, October 28. Just a few minutes ago, the HHS has released $333 million to be distributed among 10,000 Nursing Homes in our country based on the NHSN data that’s being put in weekly by the Nursing Homes. And how that ties to surveillance is if I have a robust surveillance program and Infection Control program that meets all the elements of a good quality surveillance program. So I need to have a standardized definition. That’s part of our requirements for participation. So the most commonly recognized one is McGeer criteria. So the reason why they need to have a really good baseline definition of all the different types of infections is because everybody needs to be speaking the same language. So that if you’re one person thinks that let’s just do a C. difficile, which is a common example, if a person has one of the criteria, and that infection control program says “Oh, yeah, we had a case of C. diff,” when actually the definition says you have to have two different criteria, your infection rates could be off.
And so, by monitoring and surveillance, seeing these infections, you’re preventing them by acting upon what you’re seeing in the data, you’re catching outbreaks before they’re there. They’re rampant, and what the HHS just released today is those Nursing Homes, from August to September, that showed a decrease in a significant decrease in the number of COVID-19 cases they had and the number of COVID-19 deaths they had. They’re being given these incentive payments. And so if these Nursing Homes hadn’t started doing good surveillance on their cases, and testing is part of that, testing is a very important part of surveillance. Because staff testing, which is mandated under the NHSN, now, it’s another rule regulation they have to follow, it has to be done in a certain regimented timeframe.
So either monthly, weekly, or twice a week, if these Nursing Homes weren’t doing this testing and checking in and identifying staff who perhaps are positive, which alludes to a greater community spread because the staff is the ones that are going out in the community. So if they’re coming in with positives, well, it’s probably in the community, we need to lock things down and be really strict in our buildings, which these Nursing Homes have been doing. And that’s what’s lowering their cases of COVID. They’re making sure they’re following processes those Infection Preventionist are not afraid to speak up and say “Hey, nurse Sally, you did not wash your hands properly, or you didn’t follow the right PPE that you’re supposed to, for that resident who has COVID, they’re speaking up and acting upon it. And that’s what’s lowering their cases and their death rates, and the government is giving them incentive payments for that.
Jason Long
I’m kind of curious, out of the total number of Skilled Nursing Facilities out there, what percentage you think are doing a really good job, and not really good job?
Lauri Laxton
Well, you can actually get to that data yourself. That is all publicly reported data. So you can go into the NHSN site, where they’re publicly reporting. And if you want to just look at COVID-19, Nursing Home data, you can go into that site. I’m sure will have this link for everyone here, you can go into there and see what the rates are in the different counties in your area, and then what’s going on what is being reported by the Nursing Homes. And then also, surveys are happening. Now they held up annual surveys looking at the big picture. So when a surveyor goes into a Nursing Home, they’re looking at everything from how you’re handling your food processing, in the kitchen, to the electrical systems to infection control. Well, when the pandemic started, they said “Okay, forget about everything else, let’s just focus on going there and check and see if they’re doing good infection control programs.” Well, then in the summer, they said, “Okay, we’re going to release the surveyors to look at everything.” Again, all of these surveys have what they call F-Tags that they give to the Nursing Homes that are tied to dings, you know, in their survey that they find an F880, which is the Infection Control, one that we’ve had for years, that one’s been the number one for years. But then this summer, and during the pandemic, they’ve got all kinds of new F-Tags. They have them if you’re not reporting to the NHSN, and all that kind of stuff, with all of these F-Tags and the survey results are publicly reported data than any of us can go in and look and see how the various Nursing Homes in our area and various areas of the country are doing and how much how many are being tagged on these infection control issues. So rather than me put a percentage and a guess, I would encourage people can go in themselves and look and see, I do know, it has been a problem. It has been a problem for many years because the government wouldn’t be doing such a push and so much training around infection control. I mean, we know we’ve had an issue, there have been millions of cases of hospital or healthcare-acquired in SNFs, healthcare-acquired infections for years, millions each year. And there’s been hundreds of thousands of deaths each year related to those that are occurring in Nursing Homes that are documented in many areas. And so obviously, if we’re having that many deaths, and that many infections in nursing homes, there has been a break in infection control processes. And that’s why the government’s been really hounding on it. But I think with this pandemic, it’s forced everyone to have to really “Okay, yeah, we have to follow these requirements of participation. And yes, we might get F-Tag on Infection Control, but we have people dying by the thousands, we have to get, you know, up to speed, and then with these incentive programs, it’s even going to help even more.
Jason Long
Gotcha. That’s really helpful. That’s great, great information for everybody. So when it comes to all of this, I think that there’s a lot that can be done in the way of surveillance systems, especially electronic surveillance systems. Yeah, you can talk a little bit about that.
Lauri Laxton
Well, as I’ve told you, I’ve worked for several years in the long term care field and I’ve worked with nurses who’ve done it both manually, where they have lots of sheets of paper that they’re keeping track of individual infections and testing and just writing it in logs. I’ve literally seen exit maps of the building photocopied in highlighter pens to highlight where the various infections are in the rooms. But that takes so much time. And like I said, these Infection Preventionist, they don’t have that much time, they are doing Infection Prevention and Control. But they’re also the director of nursing or they’re having to go on the floors and take care of patients as well. So those Nursing Homes around the country that I’ve also worked with who are moving to or have moved to an electronic solution, though many times there’s a little pushback in the beginning, because Oh, we’ve got to learn a new software, we don’t have time to learn the software, that time invested upfront yields tons on the back end, because everybody is entering in the data in one location. A computer obviously can sort through and filter the data much faster than a human can. These electronic solutions like Infection Watch, which ABILITY sells, it has alerts and thresholds that can be said in outbreak alerts. Like you had, you know, a nurse on the unit that reported that Mr. Jones had a cough and a fever. And then a nurse on a different floor reported this person had a cough and a fever. Well, now the Infection Preventionist can get notified, “Hey, you might have an outbreak going, you’ve got similar symptoms going on on different floors, it may be spreading throughout the building, you might want to get on it.” If I was doing that on paper manually, it would be much slower, it could be done. But I can’t even imagine the nightmare of having to go through all of that and figure it all out. Not to mention the graphs and the filtering capabilities.
And Infection Watch has a facility map, no more of those highlighter pens. Let’s say that a nurse forgot to highlight a room of somebody who had an MDRO, which is a MultiDrug-Resistant organism. If they forgot to highlight it in a color. Well, you have that risk of when you’re doing it manually, you have the risk of human error. “I forgot to color that room yellow,” well that patient discharges and the next one comes in, and he ends up with the same infection. Well, if I was notified that by color, and I didn’t realize they didn’t mark it down before, I may have missed an opportunity to go educate my environmental staff that you are not terminally cleaning the rooms between patients, whereas an electronic solution will bring that kind of stuff to the forefront, it lights it up. You had an infection last month at this and this month. Now you got the same infection. Well, two different patients What’s going on?
Jason Long
That sounds so… Having had to take things from paper into electronic formats and just having to, in the past many years ago, work just with paper. Yeah, it’s possible, but nobody does it. Because, yeah, it’s not possible having to sort through all that stuff, you pretty much just have to take it into a computer and take it from there. Anyway.
Lauri Laxton
That’s it, you take it from paper and you’re gonna have to have a transcription, you could have a transcription error, you’re going to have to put in a key computer at some point to be able to track and graph you know. Where are our peaks every year for flu? Yeah, it’s October to March, is when the flu season is, but in our building, it’s January and February each year, you know, you’d have to put that on a computer. And what’s nice about how ABILITY’s Infection Watch talks to EMRs. Like Net Solutions, this is a time saver for nurses too, because they’re already having to do MDS Assessments. And many times they’ll have a Care Watch. And then they’ll buy Infection Watch while they talk to each other and the demographic information that’s in those MDS assessments can be pulled over into Infection Watch. So when they’re going to enter an infection, they’ll have the name and then, you know, all the demographic information, age, and stuff of that resident. And they can even help with the setting up initially of your facility, like what rooms and what room is a patient in and you know, what rooms belong to what units and things like that. So there are some benefits to having it connect to an EMR where it can pull some of that information for you.
Jason Long
Okay, cool. Was there anything else where we’re gonna talk more about SNF’s QRP at all, or did we cover that pretty well?
Lauri Laxton
You know, I would like to bring that up because we brought up the announcement of the incentive payments. It just came out today. Well, CMS announced early. Well, I want to say it was probably September-ish, they announced that “Oh, we may put out a new SNF QRP measure tied to HAI’s or healthcare-acquired infections.” And then they put it in Comment Period and that comment period where everybody could comment on it. The proposed measure ended on October 14. But yes, they offered it up for comment. But then during that comment period, CMS released through the CASPER system, a dry run of the report for that new measure. So that kind of leads me to believe “Yeah, we want to hear your comments, but it’s common, whether you like it or not this new measure and it’s going to be tied to how hospitals claim.”
But then during that comment period, CMS released through the CASPER system, a dry run of the report for that new measure. So that kind of leads me to believe “Yeah, we want to hear your comments, but it’s common, whether you like it or not this new measure and it’s going to be tied to how hospitals claim.”
But one of the key points there. I actually have submitted a question to CMS, and I’m waiting to see what the answer is, is the actual definition of a healthcare-acquired infection? Because if you read the proposed measure, and… What did they call it? I think they called it the Technical Expert Panel that proposed it, the thing’s 40 or 50 pages long. But if you really read it, they said they strongly wanted to align the measure with the CDC then the NHSN time window for HAI. Okay, well, if you want to align with that definition, then you need to have the same time window. And what I mean by that is this newly proposed HAI QRP measure, specifically states that an HAI would be attributed to an SNF, starting on the fourth day after admission into the SNF, and carrying on all the way until three days after discharge, so they get discharged to the hospital-based on hospital claims, and the primary diagnosis at the hospital is going to be reporting. If that person comes down with COVID, let’s say on day two, after being admitted to the hospital, they’re going to attribute that back ending to the SNF for it. Okay, so that’s interesting because that’s 72 hours. So it doesn’t start until the fourth day in the SNF so that, you know, wherever they came from, let’s say they came from the hospital, if they don’t come down with the infection until the fourth day in the SNF, well, that’s considered an HSI for the SNF all the way till three days after discharge.
But like I said, that Technical Expert Panel, so they wanted to align with the CDC, well, if you go into the CDC and NHSN documentation, they actually have a picture where they, they show calendar days and what’s considered present on admission versus an HAI, they look at two days after admission. So a patient comes from a hospital, they are admitted to the SNF, if they come down with an infection, within day one or day two, that is going to be attributed to the hospital and day three in the SNF, now is considered an HAI in the SNF. Well, that’s a little bit different, it’s day three. So is it 48 hours? Or is it 72 hours? And that’s something I think we all need to watch for, and see if CMS specifically outlines it, because going back to all of our discussion on surveillance and everything, we need to keep track of that, of an Infection Control Program, what infections are considered HAI versus what are which are considered what we call either Present on Admission or Community-Acquired Infection. They need to know how to be able to record that in their software or if they’re doing it manually. So CMS has got to really specify what is considered an HAI. So it’s across the board the same because it would be terrible to have one definition from CDC but then a QRP measure measures in a different way.
Jason Long
It wouldn’t be the first time though.
Lauri Laxton
Exactly. So stay tuned. We’re all waiting to hear what’s going to happen.
Jason Long
All right, excellent. Well, this has been really, really informative. I’m sure that our listeners as well are gonna find this really, really informative. Thank you so much for your time today. This is incredible information. If you ever want to come back on under this video blog, and talk again, I would love to pick your brains.
Lauri Laxton
Just ask, not a problem. As you can see, I’m very passionate about Infection Control. So anytime I can be of assistance, I would love to help.
Jason Long
Perfect, thank you so much. And this article and this video will be online soon, probably within a couple of days. Okay. All right. Thank you so much. Thank you. Bye.